What is septoplasty?
Septoplasty is a surgical procedure performed to correct a deviated or crooked septum, which is the partition that separates the two nasal passages. A deviated septum can cause nasal obstruction, breathing difficulties, recurrent sinus infections, nosebleeds, and snoring.
During a septoplasty, the surgeon makes an incision inside the nose to access the septum. They then carefully remove or reshape the deviated portion of the septum, straightening it and improving the airflow through the nasal passages. In some cases, additional procedures such as turbinate reduction (reducing the size of the nasal turbinates) or nasal valve repair may be performed concurrently to optimize nasal function.
Septoplasty vs. rhinoplasty: what’s the difference?
Septoplasty and rhinoplasty are both surgical procedures that involve the nose, but they serve different purposes:
Septoplasty is a surgical procedure specifically aimed at correcting a deviated or crooked septum. Septoplasty is primarily performed to improve nasal function and alleviate symptoms such as difficulty breathing, nasal congestion, or chronic sinus issues caused by a deviated septum. During septoplasty, the surgeon will straighten or remove the deviated portion of the septum to improve airflow and restore proper nasal function. Septoplasty is typically considered a functional procedure rather than a cosmetic one.
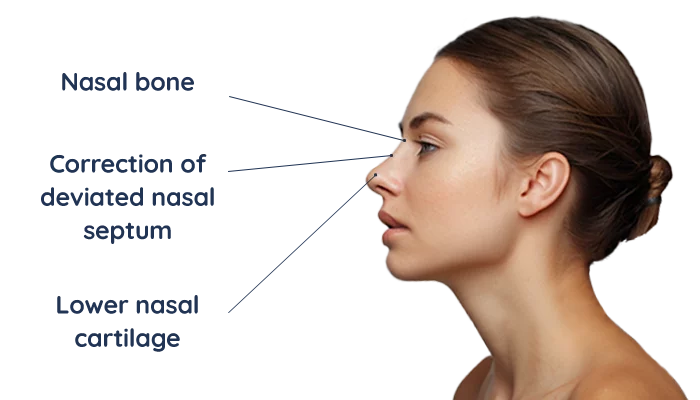
Rhinoplasty, on the other hand, is a surgical procedure that focuses on reshaping and altering the external appearance of the nose for aesthetic purposes. It can also address functional issues if needed. Rhinoplasty can involve modifying the nasal bones, cartilage, and soft tissues to achieve the desired cosmetic outcome. The procedure can address concerns such as a dorsal hump, nasal tip refinement, nostril size, or overall nose proportions. Rhinoplasty can be performed for purely cosmetic reasons or to improve both the appearance and function of the nose.
While septoplasty and rhinoplasty can be performed individually, they can also be combined in some cases. This is known as septorhinoplasty, where both the functional correction of a deviated septum and the cosmetic enhancement of the nose are addressed simultaneously.
Who are candidates for septoplasty?
Candidates for septoplasty are individuals who have a deviated or crooked septum that is causing significant functional issues and symptoms. Some common indications for septoplasty include:
- Nasal obstruction: If a deviated septum is causing persistent nasal congestion and difficulty breathing through the nose, despite conservative treatment measures such as nasal sprays or decongestants, septoplasty may be considered.
- Chronic sinusitis: A deviated septum can obstruct proper sinus drainage, leading to recurrent sinus infections, sinus pressure, facial pain, and frequent episodes of sinusitis. Septoplasty may be recommended in cases where the deviated septum contributes to chronic sinus issues.
- Nasal airflow issues: Individuals experiencing persistent nasal airflow issues, such as snoring, mouth breathing, or sleep apnea, that are associated with a deviated septum may benefit from septoplasty to improve their breathing patterns and quality of sleep.
- Nasal trauma: Trauma or injury to the nose can result in a deviated septum. If the deviation is causing significant functional impairment or symptoms, septoplasty may be performed to correct the deviation and restore proper nasal function.
- Chronic nosebleeds: A deviated septum can lead to dryness, irritation, and frequent nosebleeds. In cases where conservative measures fail to address the issue, septoplasty may be considered to alleviate the nosebleeds.
It is important to note that not all individuals with a deviated septum require septoplasty. The decision to undergo septoplasty should be made after a thorough evaluation by an ENT specialist or facial plastic surgeon who can assess your specific nasal condition, evaluate your symptoms, and determine if septoplasty is the appropriate treatment option for you. They will consider factors such as the severity of the deviation, the impact on nasal function, and the potential benefits and risks of the procedure.
How is septoplasty performed?
Septoplasty is a surgical procedure that is typically performed by an ENT (ear, nose, and throat) specialist or a facial plastic surgeon. Here is a general overview of how septoplasty is performed:
- Anesthesia: Septoplasty can be performed under either general anesthesia or local anesthesia with sedation, depending on the surgeon's preference and the patient's needs.
- Incision: The procedure begins with the surgeon making an incision inside the nose. This incision is typically made on one side of the nasal septum, which is the partition that separates the two nasal passages.
- Accessing the septum: After the incision is made, the surgeon carefully lifts the nasal lining to gain access to the deviated septum.
- Reshaping or removal: The surgeon then proceeds to reshape or remove the deviated portion of the septum using various surgical instruments. The goal is to straighten the septum and improve the airflow through the nasal passages.
- Nasal packing or splints: In some cases, nasal packing or splints may be placed inside the nose temporarily to provide support to the septum during the initial healing phase. These packing materials are typically absorbable and do not need to be removed.
- Closure and recovery: Once the necessary adjustments to the septum are made, the surgeon closes the incision with dissolvable sutures. The surgeon may also place external nasal splints to help maintain the shape of the nose during the healing process.
- Post-operative care: After the procedure, patients are usually monitored in a recovery area for a short period. They are then provided with instructions on post-operative care, which may include guidelines for nasal hygiene, pain management, and follow-up appointments.
The duration of a septoplasty procedure can vary depending on the complexity of the deviation and any additional procedures performed simultaneously. Typically, the surgery takes around one to two hours.
It is important to note that the specific details and techniques used during septoplasty may vary depending on the surgeon's expertise and the individual patient's needs. It is advisable to consult with a qualified medical professional who can provide personalized information and guidance based on your specific condition.
How to prepare for septoplasty
Before undergoing septoplasty, it is important to follow the pre-operative instructions provided by your surgeon. Here are some general guidelines to help you prepare for septoplasty:
- Consultation and medical history: Schedule a consultation with your surgeon to discuss your medical history, any medications you are taking, and any pre-existing health conditions. Provide accurate information about any allergies, previous surgeries, or bleeding disorders.
- Medications: Inform your surgeon about all medications you are currently taking, including prescription medications, over-the-counter drugs, and supplements. Your surgeon may provide instructions on which medications to continue or discontinue before the surgery, including blood-thinning medications that may increase the risk of bleeding.
- Smoking and alcohol: If you smoke, it is advised to quit smoking before the surgery, as smoking can impair healing and increase the risk of complications. Avoid consuming alcohol for a few days before the surgery as well, as it can interfere with anesthesia and recovery.
- Fasting: Your surgeon will provide instructions on fasting before the surgery. Typically, you will be asked to avoid eating or drinking anything, including water, for a specific period of time before the procedure.
- Arrange transportation and support: Since septoplasty is performed under anesthesia, it is important to arrange for someone to drive you home after the surgery. It is also helpful to have someone available to assist you during the initial recovery period.
- Pre-operative testing: Your surgeon may order pre-operative tests, such as blood work or imaging, to assess your overall health and the specific condition of your nose. Follow any instructions regarding these tests and ensure they are completed before the surgery.
- Recovery preparation: Before the surgery, prepare your home for the recovery period. Stock up on necessary supplies, such as clean gauze, saline nasal spray, pain medications (if prescribed), and soft foods that are easy to eat during the initial recovery period.
- Follow instructions: It is crucial to carefully follow the pre-operative instructions provided by your surgeon. These instructions may include guidelines on showering, avoiding certain skincare products or makeup, and avoiding food or drink on the day of surgery.
Remember to reach out to your surgeon if you have any questions or concerns during the preparation process. They will provide you with personalized instructions based on your specific needs and medical history.
What is the recovery like?
The recovery process after septoplasty can vary from person to person, but here are some general aspects of what to expect:
- Post-operative care: Your surgeon will provide specific instructions on how to care for your nose after the surgery. This may include guidelines on cleaning the incision site, using saline nasal sprays or rinses, and avoiding activities that can put strain on your nose, such as heavy lifting or strenuous exercise.
- Nasal packing and splints: In some cases, your surgeon may place nasal packing or splints inside your nose to support the septum during the initial healing phase. These packing materials are typically absorbable and do not require removal. If external nasal splints are placed, they are usually removed within a week.
- Swelling and bruising: Swelling and bruising around the nose and eyes are common after septoplasty. This tends to peak within the first few days and gradually subsides over the following weeks. Applying cold compresses and keeping your head elevated can help reduce swelling.
- Pain and discomfort: Mild to moderate pain or discomfort is normal after septoplasty. Your surgeon may prescribe pain medication or recommend over-the-counter pain relievers to manage any discomfort. Follow your surgeon's instructions on medication usage.
- Nasal congestion and drainage: It is common to experience nasal congestion, stuffiness, and a feeling of nasal drainage after septoplasty. Your surgeon may recommend using saline nasal sprays or rinses to keep the nasal passages moist and to help remove any crusts or dried blood.
- Activity restrictions: Your surgeon will provide specific instructions regarding activity restrictions. In general, it is important to avoid strenuous activities, heavy lifting, and activities that can increase blood pressure for a few weeks after the surgery. Gradually resume normal activities as advised by your surgeon.
- Follow-up appointments: You will have follow-up appointments with your surgeon to monitor your healing progress. These appointments allow your surgeon to assess the results, remove any packing or splints if necessary, and address any concerns or questions you may have.
- Recovery time: The recovery time can vary, but most individuals can expect to resume normal daily activities within one to two weeks after septoplasty. However, it may take several weeks or even months for the full healing and final results to be achieved.
It is important to closely follow your surgeon's post-operative instructions and attend all scheduled follow-up appointments to ensure a smooth recovery. If you experience severe pain, excessive bleeding, difficulty breathing, or any other concerning symptoms, contact your surgeon immediately.
Potential risks and complications
Like any surgical procedure, septoplasty carries potential risks and complications. While these risks are generally rare, it is important to be aware of them before undergoing the surgery. Some possible risks and complications of septoplasty include:
- Bleeding: Some amount of bleeding is expected after septoplasty, but significant bleeding is rare. In rare cases, it may require additional medical intervention such as nasal packing or surgical intervention to control the bleeding.
- Infection: Although infection is uncommon after septoplasty, there is a small risk. Your surgeon may prescribe antibiotics to minimize this risk. Signs of infection may include increased pain, persistent fever, worsening swelling, or discharge that is foul-smelling or discolored.
- Septal perforation: In rare cases, the septum may develop a hole or perforation as a result of septoplasty. This can lead to symptoms such as whistling sounds during breathing, crusting, and nasal discomfort. Septal perforation may require additional treatment or surgical repair.
- Changes in nasal shape or sensation: Septoplasty is primarily performed to improve nasal function, but it can also have a slight impact on the external appearance of the nose. In rare cases, there may be changes in nasal shape, symmetry, or sensation. It is important to discuss any aesthetic concerns with your surgeon before the procedure.
- Scarring: Septoplasty is typically performed using internal incisions, so visible scarring is minimal. However, in some cases, external incisions or additional procedures may result in more noticeable scarring.
- Nasal obstruction recurrence: While septoplasty aims to correct the deviated septum and improve nasal airflow, there is a possibility of recurrence of nasal obstruction over time. This can occur due to factors such as natural healing processes, nasal trauma, or the development of new nasal issues.
- Anesthesia-related risks: Septoplasty is performed under either general anesthesia or local anesthesia with sedation. Both types of anesthesia carry their own set of risks, including allergic reactions, breathing difficulties, or adverse reactions to medications. Your anesthesiologist will discuss these risks with you before the surgery.
It is important to discuss these potential risks and complications with your surgeon before undergoing septoplasty. They will be able to provide you with personalized information based on your specific situation, address any concerns you may have, and help you weigh the risks against the potential benefits of the procedure.
Cost
The cost of septoplasty can vary depending on various factors such as the geographical location, the surgeon's experience, the complexity of the procedure, the surgical facility, and any additional procedures or tests required. It is important to note that the following information provides a general idea of the cost and may not reflect the actual cost in your specific situation.
In the United States, the average cost of septoplasty can range from around $3,000 to $10,000 or more. This cost typically includes the surgeon's fee, anesthesia fees, facility fees, pre-operative testing, and post-operative care. However, it may not cover additional costs such as medications, follow-up appointments, or any potential complications that require further treatment.
It is also worth noting that insurance coverage for septoplasty varies. In cases where septoplasty is performed to address functional issues and improve breathing, insurance may partially or fully cover the cost. However, coverage is typically dependent on medical necessity, and it is important to check with your insurance provider to understand your specific coverage and any pre-authorization requirements.
To determine the exact cost of septoplasty in your case, it is best to consult with a qualified surgeon or their office. They will be able to provide a more accurate estimate based on your individual circumstances and insurance coverage, if applicable. Additionally, they can guide you through the financial aspects and potential payment options available to you.
Septorhinoplasty
Septorhinoplasty, also known as rhinoseptoplasty, is a combined surgical procedure that involves both functional and cosmetic aspects of the nose. It combines the functional correction of a deviated septum (septoplasty) with the aesthetic enhancement of the external appearance of the nose (rhinoplasty).
During rhinoseptoplasty, the surgeon addresses both the functional issues related to a deviated septum and any cosmetic concerns the patient may have. The procedure is typically performed by an ENT (ear, nose, and throat) specialist or a facial plastic surgeon.
The functional component of the procedure focuses on correcting a deviated or crooked septum to improve nasal airflow and alleviate symptoms such as difficulty breathing, nasal congestion, or chronic sinus issues. The surgeon straightens or removes the deviated portion of the septum, allowing for better airflow through the nasal passages.
Simultaneously, the cosmetic component of rhinoseptoplasty aims to enhance the external appearance of the nose. This may involve reshaping the nasal bones, cartilage, and soft tissues to address concerns such as a dorsal hump, nasal tip refinement, nostril size, or overall nose proportions. The surgeon works to achieve a balanced, harmonious, and aesthetically pleasing nasal appearance while considering the patient's individual facial features and desired outcomes.
Rhinoseptoplasty requires a comprehensive understanding of both functional and aesthetic aspects of the nose. It is a complex procedure that requires careful planning, precise surgical techniques, and consideration of individual patient factors.
FAQs
Can I have cosmetic rhinoplasty and septoplasty simultaneously?
Yes, it is possible to have cosmetic rhinoplasty and septoplasty performed simultaneously. This combined procedure is known as rhinoseptoplasty or septorhinoplasty. Rhinoseptoplasty allows for the correction of both functional issues related to a deviated septum and cosmetic concerns of the nose in a single surgical session. During the procedure, the surgeon will address the functional aspects of the nose by straightening or removing the deviated portion of the septum to improve nasal airflow and alleviate symptoms such as difficulty breathing or nasal congestion. At the same time, the surgeon can also reshape the external appearance of the nose to address cosmetic concerns, such as a dorsal hump, nasal tip refinement, or overall nose proportions.
Does septoplasty help with snoring?
Septoplasty can potentially help with snoring, but it depends on the underlying cause of the snoring. Snoring is often caused by the vibration of soft tissues in the throat or nasal passages due to airflow obstruction. While septoplasty primarily focuses on correcting a deviated septum, which is the partition between the nasal passages, it can indirectly improve nasal airflow, which may alleviate snoring in some cases.
When can I blow my nose after septoplasty?
You should avoid blowing your nose for at least one week or as directed by your surgeon following septoplasty.
Can a deviated septum be corrected without surgery?
While non-surgical options exist to manage symptoms associated with a deviated septum, such as medications, nasal dilators, and nasal irrigation, these methods cannot correct the actual deviation of the septum itself. Septoplasty surgery is typically the recommended treatment to correct a deviated septum and provide long-term relief.