What are dental implants
Dental implants, also known as tooth implants, are artificial tooth roots that are surgically placed into the jawbone to support a replacement tooth or a dental bridge. They are a popular and effective long-term solution for replacing missing teeth. Dental implants provide a strong foundation for the replacement teeth and offer several advantages over other tooth replacement options.
The implant itself is typically made of biocompatible materials, such as titanium, that fuse with the jawbone through a process called osseointegration. This integration ensures stability and durability for the implant. Dental implants can be used to replace a single tooth or multiple teeth, or even provide support for full dentures.
Dental implants offer numerous benefits, including improved appearance, speech, and chewing function. They are designed to look, feel, and function like natural teeth, providing patients with increased confidence and comfort. Additionally, dental implants are known for their long-term success, with proper care and maintenance.
Why are dental implants used?
Dental implants are used for various reasons and offer several advantages over other tooth replacement options. Here are some benefits of dental implants:
- Tooth replacement: Dental implants are primarily used to replace missing teeth. Whether a single tooth is missing or multiple teeth are lost, implants provide a stable and long-term solution. They can effectively restore a complete and natural-looking smile.
- Improved function and chewing: Dental implants function and feel like natural teeth, allowing individuals to chew and bite with ease. Unlike removable dentures, implants provide stability and prevent slippage or discomfort while eating. This enables individuals to enjoy a wide range of foods without restrictions.
- Enhanced appearance: Missing teeth can affect a person's facial aesthetics, causing the face to appear sunken or aged. By replacing missing teeth with dental implants, the natural contours of the face can be restored, providing a more youthful and attractive appearance.
- Preservation of jawbone: When a tooth is lost, the underlying jawbone can deteriorate over time. Dental implants help stimulate the jawbone, preventing bone loss and maintaining its structure. This is crucial for preserving facial integrity and preventing further dental issues.
- Speech improvement: Missing teeth, especially in the front of the mouth, can affect speech clarity. Dental implants restore proper speech patterns and pronunciation, allowing individuals to speak confidently and clearly.
- Durability and longevity: Dental implants are designed to be a long-lasting solution for tooth replacement. With proper care and maintenance, implants can last for many years, often a lifetime. This makes them a cost-effective option in the long run.
- Comfort and convenience: Unlike removable dentures, dental implants eliminate the need for adhesives or clasps. They become a permanent part of the mouth, providing a comfortable and hassle-free solution. Implants also eliminate the inconvenience of removing and cleaning dentures.
It is important to consult with a dental professional to determine if dental implants are the appropriate treatment option for your specific needs. They can evaluate your oral health, jawbone density, and overall suitability for the procedure.
Types of dental implants
There are several types of dental implants available, each designed to address specific dental needs and anatomical considerations. The main types of dental implants include:
Endosteal Implants
Endosteal implants are the most common type of dental implants. They are placed directly into the jawbone through a surgical procedure. These implants are typically made of titanium and resemble small screws or cylinders. Once the implant integrates with the bone (osseointegration), a prosthetic tooth or crown is attached to the implant. Endosteal implants are suitable for patients with sufficient jawbone density and height.
Subperiosteal implants
Subperiosteal implants are an alternative for patients who have insufficient jawbone height or density for traditional endosteal implants. Instead of being inserted into the jawbone, subperiosteal implants are placed on or above the jawbone, just below the gum tissue. A metal framework is used to support the implant, and the prosthetic tooth is attached to it. Subperiosteal implants are custom-made based on the individual's jawbone structure.
All-on-4 implants
The All-on-4 dental implant technique is used to replace a full arch of teeth. It involves the placement of four implants strategically in the jawbone to support a full arch fixed bridge. This technique provides a stable and functional solution for patients who have lost all or most of their teeth. All-on-4 implants offer the advantage of immediate teeth replacement and reduced need for bone grafting.
Zygomatic implants
Zygomatic implants are specialized implants used when there is severe bone loss in the upper jaw, and traditional implants cannot be placed. Instead of being anchored in the jawbone, these implants are anchored in the zygomatic bone, also known as the cheekbone. Zygomatic implants offer an alternative for individuals with extensive bone loss and provide a stable foundation for dental restorations.
Mini dental implants
Mini dental implants (MDIs) are smaller in diameter compared to traditional implants. They can be an option for patients with limited bone volume or when a less invasive procedure is desired. MDIs are often used to stabilize dentures or bridges rather than supporting individual teeth. They require less bone for placement and can be suitable for patients who are not candidates for standard-sized implants.
It is important to note that the suitability of a specific implant type depends on individual oral health, bone density, and other factors. The dental professional will evaluate your case and recommend the most appropriate type of implant based on your specific needs.
Who are dental implants suitable for?
Dental implants are suitable for many individuals who have one or more missing teeth and meet certain criteria. Here are some factors that determine the suitability for dental implants:
- Adequate jawbone density: Sufficient jawbone density is necessary to support the dental implant. The implant needs a stable foundation to integrate with the jawbone through osseointegration. If the jawbone has deteriorated significantly due to tooth loss or other factors, bone grafting or other preparatory procedures may be required to augment the bone before implant placement.
- Good oral health: Candidates for dental implants should have good oral health, including healthy gums and a low risk of gum disease (periodontal disease). It is essential to have a healthy oral environment to support the long-term success of dental implants. Any existing oral health issues, such as tooth decay or gum disease, should be addressed before implant placement.
- Overall health and healing ability: General health conditions can affect the success of dental implants. Certain systemic conditions, such as uncontrolled diabetes or autoimmune disorders, may interfere with proper healing after surgery. Candidates should have good overall health and be able to undergo the surgical procedure.
- Age considerations: Dental implants can be suitable for individuals of various ages, but the jawbone development should be complete. Implants are typically not recommended for children or adolescents whose jawbones are still growing. However, dental implants can be an option for adults of any age.
- Commitment to oral hygiene: Maintaining good oral hygiene is crucial for the long-term success of dental implants. Candidates should be committed to regular brushing, flossing, and dental check-ups. Proper oral hygiene helps prevent complications such as peri-implantitis, an inflammatory condition that affects the tissues surrounding the implant.
- Non-smokers or willingness to quit smoking: Smoking can impair the healing process and increase the risk of implant failure. While dental implants can still be successful in smokers, quitting smoking or refraining from smoking during the healing period is highly recommended to improve the chances of success.
- Expectations and commitment: Candidates for dental implants should have realistic expectations and understand that the process requires time, commitment, and follow-up care. They should be motivated to undergo the necessary procedures and maintain proper oral hygiene to ensure the long-term success of the implants.
It's important to consult with a dental professional who specializes in dental implants to determine your eligibility and suitability for the procedure. They will evaluate your oral health, perform necessary examinations, and discuss your specific case to provide personalized recommendations.
How is a dental implant procedure performed?
The dental implant procedure is typically performed in several stages and requires the expertise of a dental professional. Here is a general overview of how a dental implant procedure is performed:
1- Initial consultation and examination
The first step is a thorough examination and consultation with a dentist or oral surgeon. They will evaluate your oral health, take X-rays or CT scans of your jawbone, and discuss your dental history and expectations.
2- Treatment planning
Based on the examination results, the dental professional will develop a personalized treatment plan. They will determine the number of implants needed, their optimal placement, and any necessary preparatory procedures, such as bone grafting or tooth extractions.
3- Anesthesia or sedation
Before the implant surgery, local anesthesia is administered to numb the treatment area. In some cases, conscious sedation or general anesthesia may also be used to ensure comfort during the procedure.
4- Implant placement
During the surgery, an incision is made in the gum tissue to expose the underlying jawbone. Then, a small hole is carefully drilled into the bone in the designated area for the implant placement. The implant, usually made of titanium or a titanium alloy, is then inserted into the hole.
5- Osseointegration
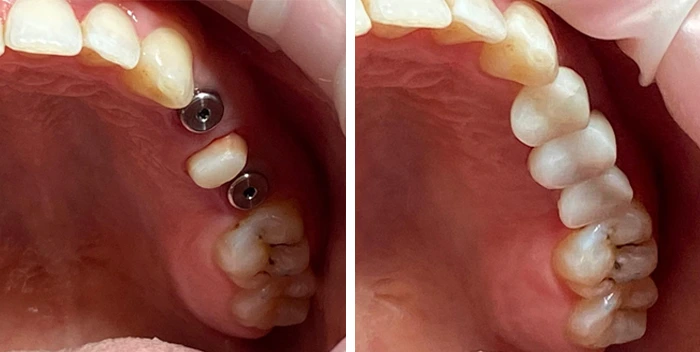
After the implant is placed, the healing process begins. Over the next few months, a process called osseointegration takes place. The jawbone fuses with the implant, creating a strong and stable foundation. During this period, a temporary crown or bridge may be placed to maintain aesthetics and function.
6- Abutment placement
Once osseointegration is complete, a minor surgical procedure is performed to attach an abutment to the implant. The abutment is a connector that protrudes above the gumline and serves as an anchor for the final restoration.
7- Final restoration
After the gums have healed and the abutment is in place, the final step is the placement of the permanent crown, bridge, or denture. This restoration is custom-made to match the color, shape, and size of your natural teeth, providing a natural-looking and functional replacement.
8- Follow-up care
After the completion of the dental implant procedure, regular follow-up visits are necessary to monitor the healing process, ensure proper function, and maintain oral health. Good oral hygiene practices, including brushing, flossing, and regular dental check-ups, are essential to the long-term success of the implant.
How to prepare for the procedure
Preparing for a dental implant procedure involves several steps to ensure that you are well-prepared both physically and mentally. Here are some important aspects to
consider when preparing for a dental implant procedure:
- Consultation and treatment planning: Schedule an initial consultation with a dental professional who specializes in dental implants. During this appointment, they will evaluate your oral health, discuss your medical history, take X-rays or CT scans of your jawbone, and develop a personalized treatment plan. This is the time to ask any questions you may have about the procedure.
- Oral health assessment: Ensure that your oral health is in good condition before the implant procedure. Schedule a thorough dental examination to address any existing dental issues, such as tooth decay or gum disease. It is important to have a healthy mouth to minimize the risk of complications during and after the implant surgery.
- Medical evaluation: Inform your dental professional about any existing medical conditions, medications you are taking, or any recent surgeries. They may request a medical evaluation to assess your overall health and determine if you are suitable for the procedure.
- Medications and supplements: Follow your dental professional's instructions regarding any medications or supplements you are currently taking. They may advise you to temporarily stop certain medications, such as blood thinners, before the surgery to reduce the risk of excessive bleeding. Always consult with your dentist and primary healthcare provider before making any changes to your medication regimen.
- Smoking cessation: If you are a smoker, it is highly recommended to quit smoking before the dental implant procedure. Smoking can impair the healing process and increase the risk of implant failure. Your dental professional may provide guidance and resources to help you quit smoking.
- Pre-operative instructions: Your dental professional will provide specific pre-operative instructions to follow before the implant procedure. This may include guidelines on fasting if general anesthesia will be used, proper oral hygiene practices leading up to the surgery, and any specific dietary or lifestyle recommendations.
- Arrange transportation and support: Depending on the type of sedation or anesthesia used during the procedure, you may need someone to drive you home afterward. Make necessary arrangements for transportation and consider having a friend or family member accompany you to provide support and assistance.
- Mental preparation: Dental implant surgery is a common and routine procedure, but it is normal to feel some level of anxiety or nervousness. Engage in relaxation techniques, such as deep breathing or meditation, to help calm your mind before the procedure. Trust in the expertise of your dental professional and the effectiveness of the treatment.
Always consult with your dental professional for personalized instructions and recommendations to ensure that you are adequately prepared for the dental implant procedure. They will guide you through the preparation process and address any concerns you may have.
Dental implant recovery and aftercare
Recovery and aftercare following a dental implant procedure are crucial for the success and long-term stability of the implants. Here are some important aspects to consider during the recovery period and for ongoing aftercare:
Short-term aftercare
- Follow post-operative instructions: Your dental professional will provide specific post-operative instructions tailored to your case. It is crucial to follow these instructions carefully to promote proper healing and minimize the risk of complications. This may include guidelines on pain management, swelling reduction, oral hygiene practices, and dietary restrictions.
- Manage discomfort and swelling: It is normal to experience some discomfort, swelling, and bruising after the dental implant procedure. Your dental professional may recommend over-the-counter pain relievers or prescribe medications to manage pain. Applying an ice pack to the outside of your face in the first 24 hours can help reduce swelling. If you experience severe or prolonged pain, contact your dentist.
- Diet and nutrition: Stick to a soft or liquid diet for the first few days following the procedure. Avoid hard, chewy, or sticky foods that can put stress on the implant site. Gradually reintroduce solid foods as advised by your dental professional. A well-balanced diet rich in vitamins and minerals will support the healing process.
- Avoid smoking and alcohol: If you are a smoker, it is strongly advised to refrain from smoking during the healing period. Smoking can impair the healing process and increase the risk of implant failure. Similarly, avoid alcohol consumption as it can interfere with the healing process and increase swelling.
- Regular follow-up visits: Attend all scheduled follow-up visits with your dental professional. These visits are crucial for monitoring the healing process, ensuring proper function, and detecting any potential issues early on. Your dentist will evaluate the implant site, make any necessary adjustments, and provide guidance on long-term care.
Remember, each individual's recovery process may vary, and it is important to consult with your dental professional for personalized aftercare instructions. By following these guidelines and maintaining good oral hygiene practices, you can help ensure the long-term success of your dental implants.
Long-term aftercare
Long-term aftercare is crucial for maintaining the health and longevity of dental implants. While dental implants are designed to be durable and long-lasting, proper care and maintenance are essential. Here are some key aspects of long-term aftercare for dental implants:
- Oral hygiene: Good oral hygiene practices are vital for the long-term success of dental implants. Brush your teeth at least twice a day using a soft-bristle toothbrush and a non-abrasive toothpaste. Pay special attention to the implant area, ensuring that you clean around the implant crown or restoration and along the gumline. Floss daily, using a floss threader or interdental brushes to clean between the implant and adjacent teeth.
- Regular dental check-ups: Schedule regular dental check-ups with your dental professional, typically every six months or as recommended. During these visits, your dental professional will evaluate the health of your dental implants, assess the surrounding tissues, and perform professional cleanings. They may also take X-rays or perform other diagnostic tests to monitor the condition of the implants.
- Professional cleanings: Regular professional cleanings are essential to remove any plaque or calculus buildup around the dental implants and ensure the health of the surrounding gum tissues. Your dental hygienist will use specialized instruments to clean the implant surfaces and provide guidance on maintaining oral hygiene at home.
- Bite and function evaluation: During regular check-ups, your dental professional will assess the bite and function of your dental implants. They will ensure that the implant-supported restoration aligns properly with the opposing teeth and that there are no issues with chewing or speaking. Any adjustments or occlusal modifications needed will be addressed to maintain proper function.
- Avoid habits that can damage implants: Avoid habits that can put excessive stress on the dental implants, such as biting on hard objects, chewing ice, or using teeth as tools. These habits can potentially damage the implant or the surrounding structures. Additionally, if you have a habit of grinding or clenching your teeth, your dental professional may recommend wearing a nightguard to protect the implants and restorations.
- Maintain overall oral health: Keeping your overall oral health in good condition contributes to the long-term success of dental implants. Follow a well-balanced diet, limit sugary and acidic foods and beverages, and avoid tobacco use. Additionally, inform your dental professional about any changes in your medical history or medications you are taking, as they may impact your oral health.
- Wear a nightguard (if recommended): If you have a habit of grinding or clenching your teeth, your dental professional may recommend wearing a nightguard to protect the implants and surrounding teeth from excessive force. This will help prevent damage and ensure the longevity of your dental implants.
By following these long-term aftercare practices and maintaining regular communication with your dental professional, you can help ensure the ongoing health and success of your dental implants. They will provide personalized guidance and address any concerns specific to your case.
Risks and complications
Like any surgical procedure, dental implant surgery carries certain risks and potential complications. While dental implant procedures are generally safe and successful, it is important to be aware of the possible risks involved. Here are some potential risks associated with dental implant surgery:
- Infection: Infection at the implant site is a possible risk. Following proper oral hygiene practices and taking prescribed antibiotics can help minimize the risk of infection. Signs of infection include persistent pain, swelling, redness, or discharge from the implant site. If you suspect an infection, contact your dental professional immediately.
- Implant failure: Although rare, dental implant failure can occur. Factors that may contribute to implant failure include inadequate osseointegration (integration with the bone), excessive forces on the implant, poor oral hygiene, smoking, or certain systemic conditions. Your dental professional will assess your suitability for dental implants and take measures to minimize the risk of implant failure.
- Nerve or tissue damage: During the implant surgery, there is a slight risk of nerve damage or injury to surrounding tissues. This can cause temporary or permanent numbness, tingling, or altered sensation in the lips, tongue, or chin. Skillful placement by an experienced dental professional reduces the risk of nerve damage.
- Sinus problems: In the case of dental implants in the upper jaw, there is a slight risk of sinus problems. If the implant protrudes into the sinus cavity, it can cause sinusitis, infection, or sinus discomfort. Proper planning and techniques, such as sinus augmentation, can minimize this risk.
- Allergic reactions: Although rare, some individuals may experience allergic reactions to the materials used in dental implants, such as titanium or certain components of the restoration. Inform your dental professional about any known allergies or sensitivities before the procedure.
- Damage to adjacent teeth or structures: During the implant placement process, there is a slight risk of damage to adjacent teeth, blood vessels, or other anatomical structures. Skillful planning, precise placement, and careful monitoring during the procedure minimize this risk.
- Complications during healing: The healing process after dental implant surgery may involve complications such as excessive bleeding, delayed healing, or poor bone integration. Following proper post-operative care instructions, maintaining good oral hygiene, and attending regular follow-up visits can help minimize these risks.
- Psychological impact: Undergoing any surgical procedure may have psychological effects, including anxiety or emotional distress. It is important to discuss any concerns or fears with your dental professional, who can provide support and guidance throughout the process.
It's important to note that while these risks exist, they are relatively rare, and the majority of dental implant procedures are successful with minimal complications. By selecting a qualified and experienced dental professional, following proper aftercare guidelines, and maintaining good oral hygiene, you can help minimize the risks and increase the chances of a successful outcome.
Cost and insurance coverage
The cost of dental implant procedures can vary depending on various factors, including the number of implants needed, the complexity of the case, the location, and the specific dental professional performing the procedure. Generally, dental implant treatment tends to be more expensive than other tooth replacement options due to the advanced technology, materials, and expertise required.
The cost of a single dental implant can range from $1,500 to $6,000 or more. This cost typically includes the implant placement surgery, the abutment (connector) placement, and the crown or restoration that attaches to the implant. Additional procedures such as bone grafting or sinus augmentation, if required, may incur additional costs.
It is important to note that the initial cost of dental implants may seem higher compared to other tooth replacement options such as dentures or bridges. However, dental implants offer long-term benefits, durability, and a more natural appearance, making them a worthwhile investment for many individuals.
Insurance coverage for dental implants varies depending on the insurance provider and the specific policy. Traditional dental insurance plans may provide coverage for certain aspects of the dental implant procedure, such as the crown or restoration, but may not cover the entire cost of the implant itself. It is important to review your insurance policy or contact your insurance provider directly to understand the extent of coverage for dental implants.
Some dental insurance plans may have waiting periods, exclusions, or limitations related to dental implants. Additionally, there may be a maximum coverage limit per year or a requirement for pre-authorization before undergoing the procedure. It is advisable to consult with your dental professional and insurance provider to determine the coverage and any out-of-pocket expenses you may incur.
Ultimately, it is important to consult with your dental professional to obtain a detailed cost estimate, discuss insurance coverage, and explore available payment options. They can help guide you through the financial aspects and provide information specific to your situation.
FAQs
How many visits do I need for a single dental implant placement?
The number of visits required for a single dental implant placement typically ranges from two to three visits.
Does dental implant surgery hurt?
Dental implant surgery is typically performed under local anesthesia, meaning the area being treated is numbed, and you should not feel pain during the procedure.
Are dental implants permanent?
Dental implants can be considered a long-term and potentially permanent solution for tooth replacement with proper care and maintenance.
Do I have an implant for each missing tooth?
In most cases, a dental implant is placed for each missing tooth. However, in some situations, multiple missing teeth can be replaced with fewer implants using techniques like implant-supported bridges or implant-supported dentures. The number of implants required depends on individual circumstances.
Are dental implants suitable for old people?
Yes, dental implants can be suitable for older individuals as long as they have good oral and overall health. Age itself is not a limiting factor, but other health considerations and bone density may be assessed to determine candidacy for dental implants.
Is it possible for a dental implant to come out or break?
While rare, dental implants can fail or experience complications such as implant fracture, loosening, or peri-implantitis. These issues can arise due to factors like poor oral hygiene, excessive biting forces, or underlying health conditions. Regular check-ups and proper care can minimize the risk of such complications.
Can children or teens get dental implants?
Dental implants are generally not recommended for children or teens since their jaws are still growing and developing. Implant placement is typically considered after jaw growth is complete. Alternative tooth replacement options may be explored for younger individuals with missing teeth.
How long does it take for the implant to fuse with the jawbone?
The process of osseointegration, where the implant fuses with the jawbone, typically takes around 3 to 6 months. However, the exact time can vary depending on individual healing abilities, bone quality, and other factors.
How soon after getting a dental implant can I eat normally?
After getting a dental implant, it is recommended to follow a soft food diet for the first few days to allow for proper healing. Gradually, you can transition to a normal diet as advised by your dental professional, typically within a few weeks.